Jump to Article
Sponsoring Institution
Program
GME Office / Administration
Finance / Public Policy

Sponsoring Institution
By: Amy Durante, MHA Amy@PartnersInMedEd.com
GMEC – Oversharing, Overthinking but Underperforming
Over the years the Graduate Medical Education Committees (GMEC) have evolved and grown into
committees with more voting as well as non-voting members. While this has its benefits as more
individuals are then privy to information firsthand, it also comes with its drawbacks. More and more Sponsoring Institutions are receiving citations from the ACGME related to lack of oversight as their GMEC minutes reflect more of an “informational dump”. Additionally, based on these citations, it appears as though the ACGME would ideally like to see the GMEC go back to its roots and become a more collaborative group meeting where true oversight of the Sponsoring Institution and programs can actually take place.
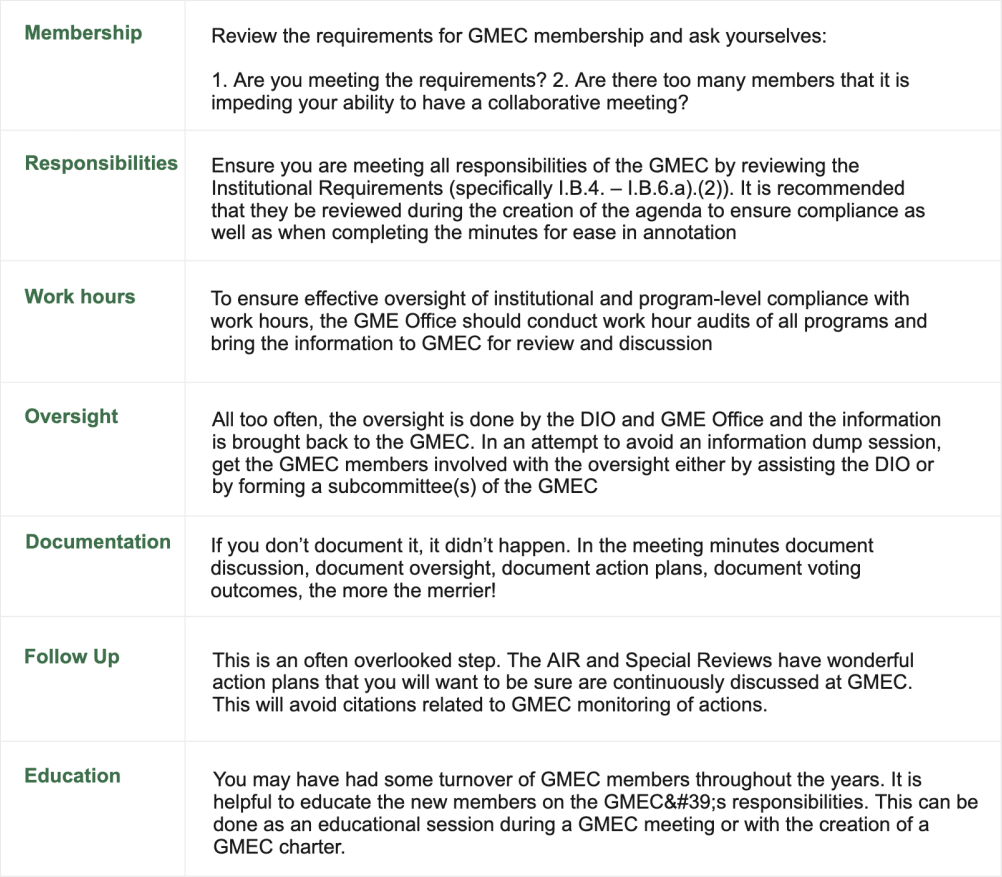
To rectify this issue and in attempts to avoid citations, the following are a few strategies that can be implemented to improve your GMEC, your oversight as well as your agenda and minutes:

Program
By: Carmela Meyer, MBA, EdD Carmela@PartnersInMedEd.com
Strategic plans aren’t just for the C-Suite
In the words of Lewis Carroll, “If you don’t know where you’re going, any road will get you there.” Many organizations (GME included) spend a significant amount of time developing a fantastic strategic plan that does not lead to the transformative change anticipated. This further leads to demotivation and frustration for those involved in the strategic planning process. The sentiment becomes “why bother, nothing ever changes.”
Why does this happen?
-
- Staying true to the mission: The mission statement, while often overlooked as a critical piece of the strategic plan, is the foundation for everything; curriculum, QI initiatives, resident/fellow recruitment and faculty development for starters. The mission statement should identify who you are at your core. To say, “We will develop strong physicians to care for our community;” is so vague and doesn’t differentiate you from any other GME program. Your mission needs to be a strong statement, it defines who you are.The three parts of a mission statement include what a program does, the program’s purpose (what it wants to achieve), and its values or how it wants to achieve those goals. The mission should also align all components of the program. For example, if your mission statement focuses on developing community physicians to address the availability of physicians, but your block diagram focuses on inpatient services and developing research, there is a misalignment between your mission and the operationalization of the mission.
- The mission’s operationalization is the plan’s strategic initiative. When these are misaligned, change becomes difficult. This is why a strong, accurate mission is critical to the success of any organization. Create 3-5 key strategic initiatives that will guide the program toward the mission. This allows programs to focus priorities and resources on a few key initiatives.
- Don’t try to solve the world’s problems in one day. A strategic plan should consider a 5–7-year span of time. The action items need to be clearly identified keeping in mind that the individuals that will implement the action item are not sitting in the room and not hearing all the discussion that has led to this point. Breaking down each initiative into component parts takes time and a systems perspective.Programs have many moving parts and impact many departments and divisions. Understanding how the program impacts other areas allows the program to maximize resources. It also allows programs to enlist support from outside the program, creating a greater likelihood for sustained change.
- Whose priority is it? Developing a sponsoring institution’s (SI) strategic plan is going to be different than a program’s plan. However, the program’s plan should support the SI’s plan. Personal preferences and passions should be open for discussion. The ultimate direction of the program is set by the Program Director. Misalignment and mistrust develop if the initiatives are not supported by the majority of the program. This is challenging as there are programs that need to consider a new strategic direction to address adverse actions, new requirements, or shifts in hospital priorities.
- Build Trust through increased communication. A lack of trust and open communication creates an environment that does not support the strategic initiatives of the program. Program Leadership, with the support of the DIO, can create an environment built on trust with transparent communication. If faculty, residents/learners, and staff know the program’s strategic direction, they can create support in their areas. Without the open dialogue, it would be challenging to enlist support. We tend to work in silos. We just need to work to build bridges from the GME silo to areas such as risk management, inpatient services, community physicians, and hospital leadership.
Overcoming these challenges takes a willingness to open the planning process to include faculty, learners, staff, and leadership. Open dialogue broadens the expertise and resources to move the program forward and everyone benefits.

GME Office / Administration
By: Alfred Peters, MBA, M.Div, PhD Alfred@PartnersInMedEd.com
The Role of an ACGME GME Program Coordinator in Compiling the Annual Program
Evaluation (APE)
The Annual Program Evaluation (APE) is a critical process for Accreditation Council for Graduate Medical Education (ACGME)-accredited programs. It provides an opportunity to assess the program’s strengths, identify areas for improvement, and develop action plans. Well-done APEs create strong, dynamic programs, and weak APEs weaken programs and lack the direction needed to maintain an exceptional training environment. As a GME program coordinator, your role in compiling the APE is multifaceted and critical. You have access to data and an understanding of the mechanisms that make you invaluable to the construction of the APE.
Let’s delve into the key components.
Step 1: Identifying Current Program Citations and Areas for Improvement.
Review the ACGME Common Program Requirements and specialty-specific requirements to ensure you follow the latest version. Identify any citations, non-compliance issues, and Areas for Improvement (AFI) from previous ACGME Letters of Notification (LON). Consult the past year’s APE, PEC, and faculty meeting notes to identify what has been done to address citations and AFIs.
Step 2: Program Mission Statement and SWOT Analysis
Include the program mission statement and SWOT analysis created by the Program Evaluation Committee (PEC) and ensure alignment with ACGME goals and the program curriculum.
Step 3: Analyzing Trainee and Faculty Surveys
Collect and analyze data from the ACGME trainee and faculty surveys. Include any additional internal survey data you may of collected. Summarize key findings, including strengths and areas for growth. Highlight any trends or recurring themes. Cut and paste 3-year trends into the APE for reference.
Step 4: Faculty Development Activities
Compile a list of faculty development activities conducted over the past year. Include workshops, conferences, and mentoring programs. Assess their impact on faculty performance and teaching effectiveness.
Step 5: Well-Being and Diversity
Gather information on resident well-being initiatives. Evaluate diversity and inclusion efforts within the program. Consider mental health support, work-life balance, and cultural competency.
Step 6: Trainee Performance Metrics
Aggregate trainee performance on in-training exams and milestones. Include pass rates and trends over the past three years. Compare results to national benchmarks. Also consider sub-specialty areas that are declining. Does this relate to faculty turnover/hires? Assess trainee progress toward milestones. Highlight achievements and areas needing to be addressed in the APE.
Step 7: Quality Improvement and Patient Safety.
Update the past year’s list of quality improvement projects and patient safety initiatives. Describe outcomes and any changes implemented. How was GME involved/impacted? Discuss how these efforts align with past action plans and ACGME requirements.
Step 8: Scholarship and Research.
Document any scholarly activities by trainees and faculty. Include publications, presentations, and research projects. Emphasize contributions to the field.
Step 9: Update Past Action Plans
Update the prior academic year’s action plan, goals, and outcomes. Identify goals that were achieved, which action plans were completed, which were not completed, and which are ongoing.
As an ACGME GME program coordinator, your role in compiling the APE is pivotal. By meticulously gathering data, analyzing trends, and collaborating with stakeholders, you contribute to program excellence and continuous improvement. Remember that the APE is not just a compliance exercise—it’s an opportunity to enhance the educational experience for trainees and promote patient care quality. Use the Partners APE template to ensure your data is complete, and the APE is comprehensive.
Finance / Public Policy
By: Heather Peters, M.Ed, Ph.D Heather@PartnersInMedEd.com
Updated GME Development Requirements for Osteopathic Colleges of Medicine (COM) Accreditation – How Does this Benefit GME?
In the past, COMs needed to document a level of engagement in creating new GME positions to absorb their COM graduates into the GME pipeline.
This expectation has ratcheted up to a new level as the GME pipeline continues to shrink.
How does this benefit GME?
For new COMs, the expectation is to demonstrate “an understanding of the obligations to ensure student entry into graduate medical education (GME) upon graduation from the proposed COM. A proposed COM must demonstrate a plan to support development and growth of GME through establishment of a GME office with qualified personnel, expertise, and financial support focused on supporting new and established GME and osteopathic recognition.” (see Candidate Standard 10: Graduate Medical Education (GME) Element 10:1: GME Feasibility)
If you have a developing COM in your area, consider a partnership with them as this can be a very beneficial relationship. COMs can provide resources (library, faculty development, and simulation center access to name a few) and funding for new programs and/or expansion of existing core programs.
Feasibility studies, a frequent activity in GME development, 1) can be funded by the COM or 2) agree to share costs. Here is the language about feasibility studies: “Provide a feasibility study outlining available GME capacity including development costs and a plan outlining how the proposed COM will ensure sufficient residency positions (PGY-1) to equal the requested class size.” (see Candidate Standard 10: Graduate Medical Education (GME) Element 10:1: GME Feasibility)
For established COMs, when they want to increase class size, they will also have to demonstrate increased GME development activity.
For more information, see accreditation standards document: https://osteopathic.org/wp-content/uploads/2023-COM-New-and-Developing-Accreditation-Standards.pdf
Or the COM Directory with contact information: https://osteopathic.org/wp-content/uploads/2018/03/colleges-of-osteopathic-medicine.pdf
Or contact the Accreditation Dean at your local COM
Is there a GME Feasibility Study in your future? Contact Partners to discuss your needs with a seasoned GME consultant.
 |
 |
 |