Jump to Article
Sponsoring Institution
Program
GME Office / Administration
Finance / Public Policy

Sponsoring Institution
By: Heather Peters, M.Ed, PhD Heather@PartnersInMedEd.com
The Three Pillars of the National Community of Sponsoring Institutions (NLCSI):
Last September, ACGME held their inaugural meeting focused on the needs of institutional representatives across GME in Chicago. The NLCSI is “designed to advance three pillars and associated domains” through “shared educational experiences, explore successful practices, and address challenges in advancing and optimizing GME.” (https://www.acgme.org/meetings-and-educational-activities/courses-and-workshops/national-learning-community-of-sponsoring-institutions-meeting/)
The three pillars of the NLCSI:
1) Demonstrating Commitment to Excellence in Patient Care;
2) Optimizing Health Systems for Learning; and
3) Transforming Education through GME Innovation.
These pillars evolved out the work of the Sponsoring Institution 2025 (SI2025) found at https://www.acgme.org/initiatives/sponsoring-institution-2025/. For those readers who are not familiar with this report, here is a brief description of this guiding document for GME strategic planning.
After a listening tour across the United States that involved over 1,000 persons, the SI2025 Taks Force created a seminal report identifying eight categories and 48 specific findings. “Three forces – democratization, commoditization, and corporatization – were seen as drivers of change that appear to be guiding the future of health care, and thereby shaping the conditions to which GME and Sponsoring Institutions will need to adapt.” https://www.acgme.org/initiatives/sponsoring-institution-2025/
At Partners®, when we work with sponsoring institutions on their GME strategic planning, we use the SI2025 findings to inform the process. Often, we find the report – or the 2-page handout we prepared for the 2023 ACGME Annual Education Meeting (click here) – helps the C-Suite at community-based institutions understand the direction that GME will take in the coming decades.
Click here for a Partners’® resource related to the mindset shifts needed and suggested curriculum components to meet the expectations of ACGME SI 2025.

Program
By: Amy Durante, MHA Amy@PartnersInMedEd.com
Major Changes of the Common Program Requirements
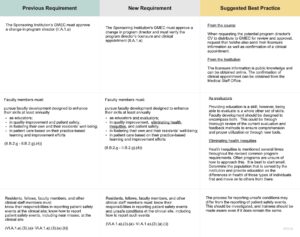
Just when you thought you had mastered all of the Common Program Requirements, the ACGME has gone ahead and updated them. If you have not had a chance to read through them during this busy onboarding season, we’ll break down a few of the major changes and provide suggestions and best practices for maintaining compliance with the new requirements.
When reviewing the new requirements, it is good practice to read the Tracked Changes version in order to decipher all of the changes, both big and small.
(Click within table to enlarge/clarity)

GME Office / Administration
By: Cheryl Haynes, BA Cheryl@PartnersInMedEd.com
Evaluate your Processes
Now that the new academic year is upon us, Program Administrators/Coordinators are wrapping up offboarding of graduates, onboarding interns, graduation, orientation planning and preparing for the transition to the new academic year. It is the busiest, most anxiety-producing time of year for Program Administration. Below are some lessons learned and suggestions for making this season a little less stressful next year.
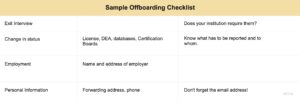
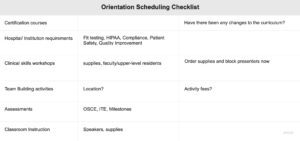
- Rehash this season. Schedule a meeting with your program administrative team now. What went well? What didn’t go so well? What should have been done differently or could have been done better? Discuss and agree now on any changes for onboarding your new trainees, for graduation, or for orientation next year. Create a checklist for each of these events, who is responsible for each task? Assign tasks as appropriate and revisit them regularly. Get started with these examples:
(Click within table to enlarge/clarity)
Lesson learned: While many programs/institutions have required prior completion of learning or training modules prior to matriculation, there is a growing trend toward compensating incoming residents for this time.
(Click within table to enlarge/clarity)
Lesson Learned: Makesure that the Graduate or Program Administration updates personal address and email address with certifying board. Information from the Board will be sent to the email address in the graduates’ profile.
(Click within table to enlarge/clarity)
Lesson Learned: Verify the need for sessions “you’ve always done.” In this day of virtual (and recorded) learning something that has taken up hours of orientation previously may easily be reduced or eliminated completely.
(Click within table to enlarge/clarity)
Lesson Learned: Is your venue large enough to accommodate the graduating class and their guests? Attendance fluctuates from year to year. Estimate attendance now. Also, don’t assume that just because graduation has taken place at the same venue for years, it will be available when you need it next year.
- Implement planned changes now. Communicate with key stakeholders sooner rather than later., e.g., who selects the guest speaker for graduation? Make that decision now and get on the person’s calendar for next year. Secure your venue. If your orientation went well and included everything required by your program and/or sponsoring institution, start planning for next year’s orientation now. Schedule appointments and get on people’s calendars.
- Have quarterly planning meetings. Don’t wait until spring to plan these events. Review and follow each of your checklists. Every task you complete and check off is one less source of stress and one less thing to do next year during the busiest and most stressful time.
- Take care of your own well-being!
Finance / Public Policy
By: Carmela Meyer, MBA, EdD Carmela@PartnersInMedEd.com
You can’t visit a news outlet without reading an article about the nursing and staffing turnover, nursing shortages at dangerous levels, and hospital service lines being closed due to the staffing shortages. This conundrum comes on the heels of a global pandemic that devastated the world. Physicians are leaving the workforce in record numbers due to increased burnout from low compensation for teaching, pressure to publish despite a lack of time and declining research funds, and a redistribution of the clinical workload. This is adding to the negative impact on the clinical learning environment. This is the environment that residents are learning to manage within their clinical learning environments.
Hospitals are managing the financial aftermath of the pandemic and the impact of historic staffing concerns. How is this impacting the learning environment of our residents? The COVID-19 pandemic resulted in restructuring didactics and clinical care based on the needs of the hospital. Data obtained from 14 pediatric subspecialties compared pre-pandemic to pandemic Subspecialty In-Training Exam scores; Infectious Diseases, Cardiology, and Critical Care Medicine saw statistically significant decreases in SITE scores.
Issues regarding resident service vs. education and supervision have been impacted by the staffing concerns of hospitals and are increasingly problematic with physician burnout and resignation. Residents are being pulled from educational experiences to help with transport, labs, and other service responsibilities.
What does all this mean for GME leaders? As leaders of the education of our future physicians we need to be protective of the education time for residents, closely guarding against using residents for patient transport or other non-physician responsibilities. As hospitals face more challenges to the safe clinical environment for the patients, we, as GME leaders, need to be just as diligent with the education time for our learners.
Banerjee G, Mitchell JD, Brzezinski M, DePorre A, Ballard HA. Burnout in Academic Physicians. Perm J. 2023 Jun 15;27(2):142-149. doi: 10.7812/TPP/23.032. Epub 2023 Jun 13. PMID: 37309180; PMCID: PMC10266848.
Thuy L. Ngo, Lisa Yanek, Derya Caglar, Jessica Bailey, Cindy G. Roskind, Melissa Langhan, Medical Knowledge Acquisition during a Pandemic: Pediatric Subspecialty In-Training Examination and Board Certification Exam Passing Rate, Academic Pediatrics, 2023, ISSN 1876-2859, https://doi.org/10.1016/j.acap.2023.05.013.
Roth, L.T., Mogilner, L., Talib, H. et al. Where Do We Go from here? Post-pandemic Planning and the Future of Graduate Medical Education. Med.Sci.Educ. 33, 375–384 (2023). https://doi.org/10.1007/s40670-023-01737-8
 |
 |
 |